TBI v MENTAL ILLNESS
TBI Survivors have a right to Neurological care.

Traumatic Brain Injury Survivors: A New Challenge for the Health Community and Public Awareness
Traumatic Brain Injury (TBI) survivors are a relatively new group within the healthcare community and society at large. Historically, individuals with severe brain injury died from the trauma. However, medical advancements pioneered during the Iraqi War have significantly  increased the survival rate for TBI patients. As a result, TBI survivors have only been a recognized presence in society for approximately 22 years. Recovery from such injuries is lengthy, often spanning 5 to 15 years. Survivors frequently experience behavioral changes due to their brain injury.
increased the survival rate for TBI patients. As a result, TBI survivors have only been a recognized presence in society for approximately 22 years. Recovery from such injuries is lengthy, often spanning 5 to 15 years. Survivors frequently experience behavioral changes due to their brain injury.
Adding to the challenge, TBI survivors are often misclassified as individuals with mental illnesses. This mischaracterization has led to misunderstandings in critical interactions with law enforcement, mental health evaluators during Temporary Detention Orders (TDOs), psychiatrists, employers, coworkers, and the general public. The symptoms of TBI—such as behavioral changes and cognitive difficulties—often mimic those of mental health disorders, making it easy to misidentify these individuals at first impression. However, TBI survivors suffer from a neurological, cognitive disability rooted in physical brain injury, not a mental illness.
Legal precedence for TBI civil rights (there are no cases) has yet to address the unique needs and rights of TBI survivors comprehensively. The lack of case law or established legal frameworks contributes to systemic misunderstandings, leaving survivors vulnerable to inappropriate treatment and discrimination.
This issue is compounded by the historical dominance of the mental health industry. Since the 3rd century, the mental state of the brain and behavior has been the primary focus, with psychiatry shaping much of our understanding. It was only in the 18th century, with the emergence of neurology, that the study of brain operations became a scientific pursuit. TBI survivors, however, have been thrust into the psychiatric domain of mental illness, when their condition belongs in the physical science domain of Neurology.
To address these gaps, society must recognize TBI survivors as individuals with distinct neurological conditions and ensure that appropriate medical, legal, and social support systems are developed to meet their needs.

Comparing the scientific definition of
Traumatic Brain Injury and Mental Illness
TBI is primarily a condition of externally induced neurocognitive dysfunction, whereas mental illnesses are defined by internally mediated disruptions in psychological and behavioral functioning. Traumatic brain injury (TBI) and mental illness represent distinct, yet occasionally overlapping conditions, each defined by specific criteria and characterized by unique etiologies and clinical presentations.
 Definition of a Traumatic Brain Injury
Definition of a Traumatic Brain Injury
CDC (Center for Disease Control) defines a traumatic brain injury as a disruption in the normal function of the brain that can be caused by a bump, blow, or jolt to the head, or a penetrating head injury. Even the DMS-5 of the American Psychiatric Association has a clear definition of Traumatic Brain Injury that describes the normal functions of the brain altered and social cognition impaired.
DSM-5 Diagnostic and Statistical Manual of Mental Disorders – TBI
Traumatic brain injury (TBI) is defined as: “brain trauma with specific characteristics that include at least one of the following: loss of consciousness, posttraumatic amnesia, disorientation and confusion, or, in more severe cases, neurological signs (e.g., positive neuroimaging, a new onset of seizures or a marked worsening of a pre-existing seizure disorder, visual field cuts, anosmia, hemiparesis. To be attributable to TBI, a neurocognitive disorder must present either immediately after the injury, or immediately after the individual recovers consciousness after the injury AND persist past the acute post-injury period. The cognitive presentation is variable. Difficulties in the domains of complex attention, executive ability, learning, and memory are common as well as slowing in speed of information processing and disturbances in social cognition. DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; May 18, 2013 by the American Psychiatric Association)
A TBI is a ripping, tearing, and shearing of brain tissue. It is a physical disability with neurological consequences in information processing, memory loss, concentration, speech, and motor control. The definition emphasizes the causal relationship between physical brain trauma, and subsequent neurocognitive dysfunction. Psychiatry is not a treatment for the loss of neural network or neurons.

Traumatic Brain Injury is considered an “Intellectual Disability” NOT a “Mental Illness” under Americans with Disability Act 1990
Definition of a Mental Illness
Federal Law Definition – 34 U.S. Code § 10472
(1) the term “mental illness” means a diagnosable mental, behavioral, or emotional disorder
(A) of sufficient duration to meet diagnostic criteria within the most recent edition of the Diagnostic and Statistical Manual of Mental Disorders published by the American Psychiatric Association; and.
(B) that has resulted in functional impairment that substantially interferes with or limits 1 or more major life activities;
DMS-5 Definition of Mental Illness or Mental Disorder:
DSM-5 consider these 5 factors:
1. A behavioral or psychological syndrome or pattern that occurs in an individual
2. Reflects an underlying psychobiological dysfunction
3. The consequences of which are clinically significant distress (e.g., a painful symptom), or disability (i.e., impairment in one or more important areas of functioning)
4. Must not be merely an expected response to common stressors and losses (ex. the loss of a loved one), or a culturally sanctioned response to a particular event (ex. trance states in religious rituals)
5. Primarily a result of social deviance or conflicts with society
“The DSM-5 will carry on the long tradition of diagnosing mental disorders using behavioral criteria alone. These criteria will continue to take the form of lists of behaviors. Biological indicators will not be used to diagnose mental disorders, because we simply don’t have the ability to do that at the moment. “(Saybrook University, What is the DSM-5 Definition of a Mental Disorder? June 7, 2017)

Comparing Traumatic Brain Injury with Psychotic Disorder
Traumatic Brain Injury
Delayed Information Processing, lack of concentration, disruption in short term memory, slowed thinking, quick to anger, mood swings, difficulty finding words.
• Speaking about what they owned
• Trouble finding words, slurred speech
• Inability to order tasks.
• Fatigue, sudden sleeping
• Inability to organize the day
• Inappropriate social skills
• PTSD from accident that caused the TBI
• Physical changes to metabolism -weight
• Speaking about their former life
Psychotic Disorder
Psychotic behavior is often categorized by its way of causing the person affected to have a skewed idea of reality.
Losing touch with reality (delusions).
Unclear and disorganized speech
Disorganized behavior
Problems sleeping
Difficulty functioning
Withdrawal from social situations.
Preoccupation with strange fears.
Change in appetite
Grandiosity
TBI Symptoms include:
Physical: headaches, dizziness, sleep problems, fatigue, light sensitivity
Cognitive: difficulty concentrating, gaps in memory, slowed thinking, difficulty finding words
Emotional: Irritability, anxiety, depression, mood swings, quick to anger.
The TBI Survivor is given a diagnosis of ‘Bipolar’ for sleeping long hours, and rushing to get things done when they are awake; ‘Depression’ for excessive sleeping 12-16 hours a day; ‘Manic’ for trying to get things done before they sleep; ‘Mood Swings’ for their irritability, and anger outbursts; “lack of impulse control” when they are “impulsive” or change their mind quickly, “outbursts” of anger, and thinking “off the top of their head” (stream of consciousness); “Schizophrenia” when they talk about their desire to regain their former life, scared of the future, and anxious to recover their skills; ‘Delusional’ thoughts of their prestige in their former life, and plans for recovering their life; “Anxiety” for fearing the future and never recovering their intellectual prowess.
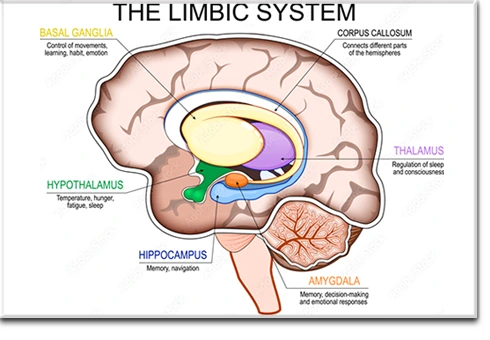 Observation: Mental health professionals often prioritize diagnosing and treating psychiatric conditions. They focus on BEHAVOIR without recognizing the underlying traumatic brain injury (TBI) affecting the survivor. Most commonly, they fail to realize it’s the LIMBIC system which is damaged, NOT a CHEMICAL IMBALANCE. The TBI Survivors behavior is NORMAL for the damaged brain, they cannot control their behavior. It is much like a child who cannot monitor their behavior until their body and mind reaches sufficient development. The emotional control mechanisms for the TBI Survivor have been damaged. It will take years for them to heal. Society must tolerate an adult with emotions like a child.
Observation: Mental health professionals often prioritize diagnosing and treating psychiatric conditions. They focus on BEHAVOIR without recognizing the underlying traumatic brain injury (TBI) affecting the survivor. Most commonly, they fail to realize it’s the LIMBIC system which is damaged, NOT a CHEMICAL IMBALANCE. The TBI Survivors behavior is NORMAL for the damaged brain, they cannot control their behavior. It is much like a child who cannot monitor their behavior until their body and mind reaches sufficient development. The emotional control mechanisms for the TBI Survivor have been damaged. It will take years for them to heal. Society must tolerate an adult with emotions like a child.
Implication: This misdiagnosis can result in inappropriate treatment plans (Medical Malpractice), including the prescription of drugs that are mood-regulating, impulse control, anti-anxiety. In some cases – the TBI Survivor faces proceedings for involuntary commitment. All stemming from a misunderstanding of the patient’s TBI-neurological impairment due to the destruction of brain tissue from the traumatic brain injury. Americans are being LOCKED UP due to a physical disability with neurological consequences.
No CHEMICAL INTERVENTION, DRUG, or LOSS of LIBERTY
will treat or cure the loss of neurons in the brain. It has also been shown that foreign substances introduced into the brain chemistry impact NEUROPLASICITY the brain’s NATURAL HEALING mechanism that repairs the neural network in the damaged area.
Medication can cause: Tardive Dyskinesia -a movement disorder that can develop if you take anti-psychotic medication. Involuntary movements – Facial muscles, tongue, neck, trunk muscles, limbs. (facial expressions, chewing, puffing your cheeks, rapid eye blinking)

A Call for Awareness
These situations highlight the critical need for greater awareness and understanding of TBI among medical professionals, the mental health community, law enforcement, the judicial system, and the public. TBI survivors face unique challenges that require compassion, tailored interventions, and recognition of their condition’s complexities. By fostering greater education and training in this area, society can help prevent unnecessary interventions, and provide more effective support for those navigating life after a traumatic brain injury.